To help doctors identify the most suitable medications for individual patients more quickly in the future, medicine is gradually adopting microchips into which various human cells are embedded - cells that respond to drug effects more rapidly than the entire human body. Researchers at Riga Technical University (RTU) are participating in a project aimed at creating joint structures on a microchip. In the European Union alone, there are nearly three million rheumatoid arthritis patients. This disease is difficult, complex, and time-consuming to treat.
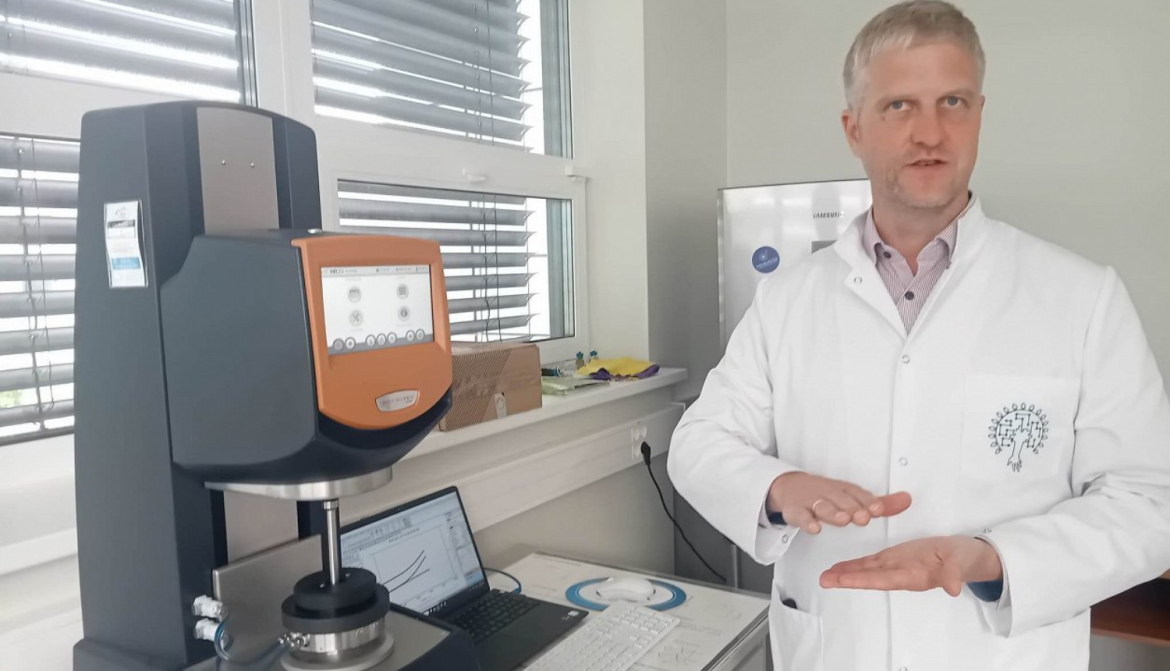
Photo: Ilze Kuzmina
"Not all patients respond well to certain medications. So, when a doctor chooses the most popular drug, or the one that usually works best, six months may pass before it's clear that the treatment is ineffective," explains Jānis Ločs, professor at RTU’s Faculty of Natural Sciences and Technologies, and project manager of the Baltic Biomaterials Centre of Excellence.
It can take a year or more to test various medications before finding one that is effective.
To shorten this treatment timeline, scientists propose testing drugs on a special microchip containing a patient’s tissue sample.
"The sample is taken, separated into cell types, then cultured and seeded into special materials that we prepare here at Riga Technical University," Ločs explains. "Our specific task in this project involves two things. First, to develop the bioink - or more precisely, a gel-based substrate- for embedding bone cells so they can grow."
Pētnieks paskaidro, ka RTU veido kaula daļas gēlu, jo jau iepriekš te pētīti materiāli kaulaudu reģenerācijai. Gēls top no ķīmiski nedaudz modificēta želatīna, kas pārveidots, lai būtu tuvāks kolagēnam. Tāpat gēlam pievienots kalcija fosfāts, kas ir kaula minerālā daļa.
Pēcāk pacienta šūnas sajauc ar šo gēlu, tad kopīgo masu, ko nu jau sauc par biotinti, pilda mikroshēmā, izmantojot īpašu 3D bioprinteri ar robota roku. To dara Šveicē, taču arī RTU ir līdzīgs bioprinteris, kurā izmanto biotinti ar dzīvām šūnām.
Ločs notes that RTU is working on creating a bone tissue gel, building on previous research in bone regeneration materials. The gel is made from chemically modified gelatin, which has been adapted to be more similar to collagen. Calcium phosphate, which is the mineral component of bone, is also added to the gel.
Next, the patient’s cells are mixed with this gel. The resulting compound- now referred to as bioink- is inserted into the microchip using a special 3D bioprinter with a robotic arm. While this procedure is currently carried out in Switzerland, RTU also has a similar bioprinter capable of using bioink with living cells.
The RTU researchers are developing these microchips as part of a large-scale project funded by the European Commission, involving 13 research institutions from 18 countries. "Everyone is pooling their strengths, and the total cost exceeds five million euros," notes Ločs.
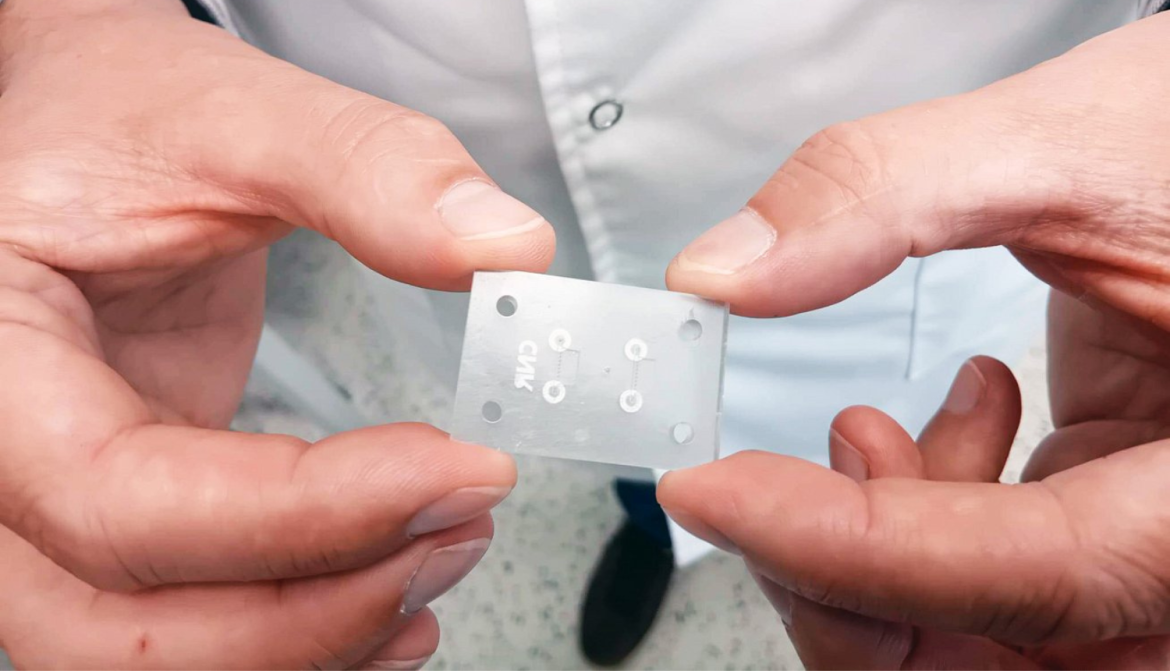
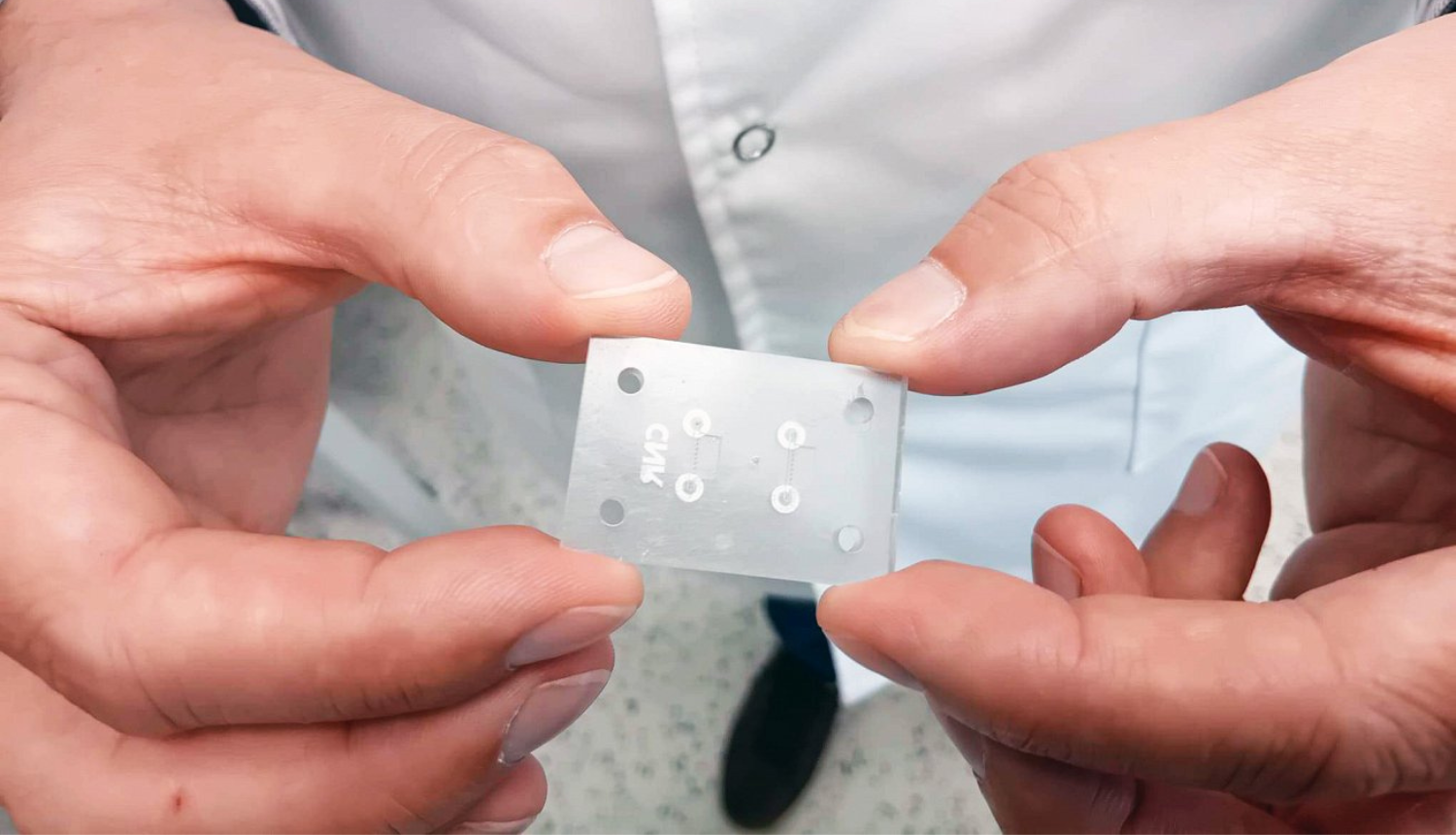
He further explains the structure of the microchip: “In the cavity, we need to place five different types of tissues - we need a blood vessel, a joint, cartilage, bone, and again a blood vessel. Using the 3D printer, we first print a gel containing blood vessel cells, then a gel with synovial cells, followed by cartilage, then bone with another blood vessel. All of this is extremely tiny - microscopic. Then we attach small tubes to it, through which fluids circulate to keep the cells alive."
All of this combined forms a microscopic artificial joint.
Researchers in each participating country have different roles. For example, in the UK, scientists are expanding patient tissue samples so they can be placed into multiple chips. Using several microchips, multiple drugs can be tested simultaneously. According to Ločs, the most effective medication could be identified within just two to three weeks this way.
In Latvia, in addition to developing the gel and bioink, researchers also test the chips using micro-CT scanning to check for any structural errors. The chip’s construction is quite complex, as the frame consists of several plates that must fit together hermetically. Glueing them is not an option, as adhesives contain solvents; therefore, they must be screwed together instead.
Another direction of the study is to simplify the chip, reducing the number of cell compartments from five to just two. This would lower costs and reduce the chances of errors during the process.
The project, which began in 2018, is set to conclude this year. Researchers are now working with real patient cells to test the efficacy of drugs using microchips.
Ločs also demonstrates how the bioprinter and its robotic arm function: “It can pick up one, two, or three cartridges. In total, you can load up to eight different cartridges, each with a different ink and needle. Then the printer is programmed to, for example, make a specific movement with the first needle, print in a specific location, set it down, pick up the next, and continue printing in sequence.”
Ločs envisions a future where such equipment could be found in operating rooms, printing the necessary tissues directly for patients. He also adds that bioprinters using bioink are at least a hundred times more expensive than regular 3D printers.